The impact of stress on sexual health By Dr. Ravi Parkash — Manodarpan Wellness, Chandigarh
- 15 Dec 2025
- stress and sexual health, stress and libido, stres...
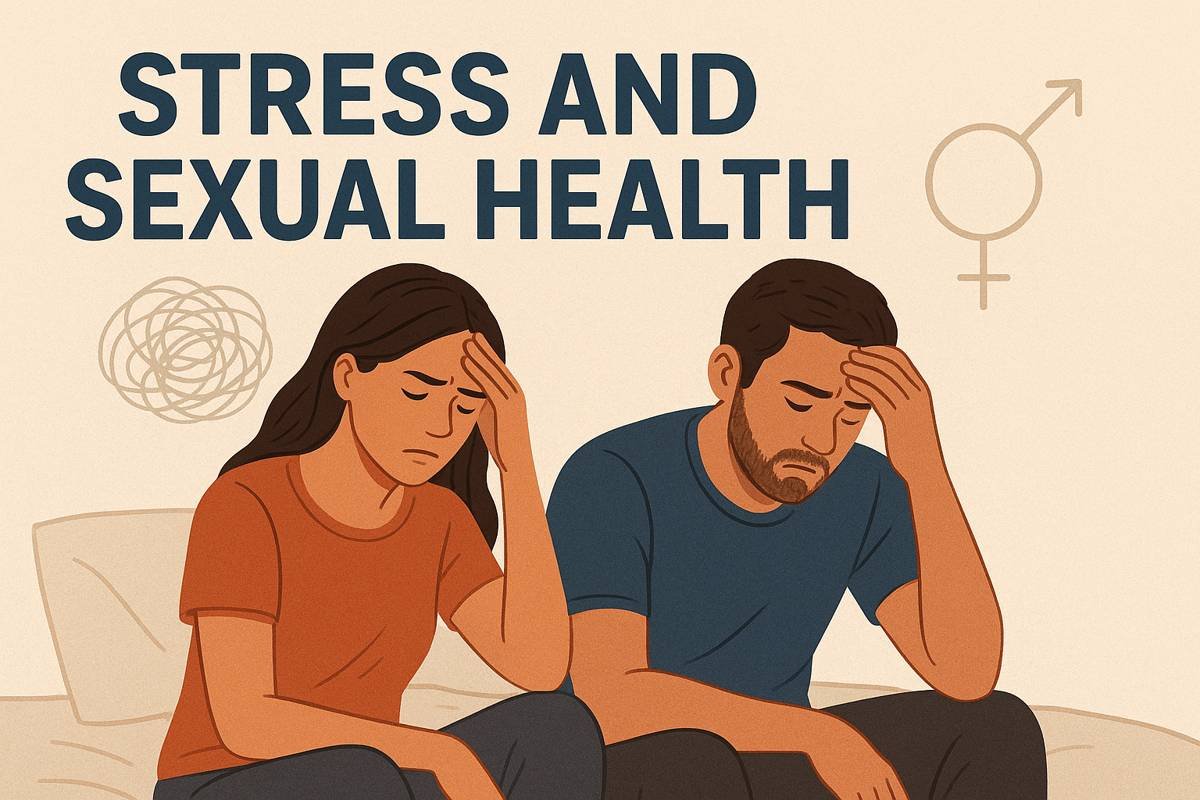
Stress is a nearly universal experience — but when stress becomes chronic, it doesn’t just make us tired or irritable. It can quietly erode sexual desire, performance, and satisfaction for both men and women. In this article, I summarise the evidence on how stress affects sexual health, explain the biological and psychological mechanisms, list common signs to watch for, and offer clear, practical steps patients can take to recover sexual wellbeing.
How stress harms sexual health — the big picture
Psychological distress (stress, anxiety, depression) is strongly associated with poorer sexual functioning and lower sexual satisfaction across populations. Studies looking at men and women consistently show that higher stress correlates with reduced desire, arousal problems, difficulty reaching orgasm, and greater sexual avoidance.
Biology: what happens in the body
-
HPA axis & cortisol: Stress activates the hypothalamic–pituitary–adrenal (HPA) axis and raises cortisol. Chronically high cortisol interferes with sex hormones (for example, it can blunt testosterone production in men) and impairs libido and erectile physiology.
-
Vascular and endothelial effects: Stress and related oxidative processes damage endothelial function, the same mechanism critical for erection (blood-flow dependent). Oxidative stress and endothelial dysfunction are well-documented contributors to erectile problems.
-
Neurotransmitters and arousal: Stress alters neurotransmitters (serotonin, dopamine, norepinephrine) that modulate sexual motivation and reward. Elevated anxiety can shift attention away from sexual cues toward threat-related thoughts, reducing arousal and increasing performance anxiety.
-
Reproductive axis disruption: Animal and human studies show chronic psychological stress can suppress gonadotropins and impair sexual behavior and fertility-related processes. While not every person exposed to stress will have these changes, prolonged exposure increases risk.
Psychological pathways — the role of the mind
Even when the body is physically capable, stress can sabotage sex via:
-
Cognitive interference: Worry and rumination during intimate moments reduce focus on pleasurable sensations.
-
Negative self-appraisal: Performance anxiety or self-criticism feeds a cycle of avoidance and rising distress.
-
Relationship spillover: Work stress, financial strain or caregiving burden reduce time, spontaneity, and emotional closeness — all important for a healthy sexual life.
Typical signs patients report
-
Decreased sexual desire or interest
-
Difficulty getting or maintaining erection (men)
-
Reduced vaginal lubrication or difficulties with arousal (women)
-
Delayed or absent orgasm, decreased sexual satisfaction
-
Avoidance of intimacy, relationship tension
If sexual problems are accompanied by persistent sadness, panic symptoms, or relationship conflict, those are important red flags to evaluate further.
What helps — evidence-based approaches
-
Address stress directly (psychological interventions). CBT, mindfulness-based stress reduction, and specific sex therapy techniques reduce perceived stress and improve sexual function in many studies. Combining psychological therapy with medical treatment often gives the best results.
-
Lifestyle measures. Sleep optimisation, regular physical activity, balanced nutrition, and limiting alcohol/tobacco help normalise hormones and vascular health — all supportive of sexual function.
-
Medical review. Screen for medical contributors (diabetes, hypertension, dyslipidaemia, endocrine disorders, medication side effects). Treating underlying medical causes can restore sexual function in many cases.
-
Couple communication & behavioural strategies. Scheduling intimate time, sensate-focus exercises, and reducing performance pressure (reframing sex as connection rather than “performance”) are practical, therapist-guided tools that reduce anxiety and rebuild desire.
A practical plan you can try
Step 1 — Screening (in clinic or self-check): Ask simple questions about sleep, mood, substance use, medications, and relationship stress. If sexual dysfunction is present for >3 months and causes distress, consider a referral.
Step 2 — Targeted interventions:
-
Short course of CBT or mindfulness for stress/anxiety; consider sex therapy for persistent sexual difficulties.
-
Review medications (antidepressants, antihypertensives) that may reduce libido and discuss alternatives.
-
Lifestyle prescription: 30 min brisk walk 5x/week, sleep hygiene, reduce alcohol/tobacco.
Step 3 — When to consider medical treatments: For men with vascular or hormonal causes, phosphodiesterase inhibitors (e.g., sildenafil) or hormone evaluation may be appropriate alongside stress management. For women, targeted treatments depend on the specific dysfunction and should be individualized.
When to seek specialist help
Seek specialist care if sexual problems are persistent (≥3 months), cause substantial distress, or are accompanied by severe mood, suicidal thoughts, or relationship violence. A biopsychosocial evaluation — combining psychiatry/psychology, urology, or gynecology as needed — provides the most effective pathway.
Final thoughts from Manodarpan Wellness, Chandigarh
Sexual health is an integral part of overall wellbeing — and stress is a common, treatable barrier. With a clear assessment, stress-focused therapy, lifestyle change, and targeted medical support when needed, most people can see meaningful improvement. If stress or sexual concerns are affecting your life, reach out — help is available, and recovery is possible.
About the author: Dr. Ravi Parkash, Consultant Psychiatrist, Manodarpan Wellness, Chandigarh. We provide confidential assessment and combined psychological-medical treatment plans for stress-related sexual difficulties.
Contact : To book a consultation at Manodarpan Wellness, Chandigarh, call our clinic or visit our website